 On the Case
On the Case
By Kevin Haines, DO, and Alex Merkulov, MD
Radiology Today
Vol. 25 No. 7 P. 30
History
A 30-year-old man presented to otolaryngology with a midline neck mass. Patient reported noticing the midline neck mass a few weeks after a viral illness. On physical exam, a 4.5 cm in diameter mass was noted just left of midline without overlying skin change. The mass was mobile with swallowing. There was no associated tenderness. The patient denied weight loss, difficulty swallowing, or other constitutional symptoms. The patient was referred for a soft tissue targeted neck ultrasound and a CT of the neck with IV contrast.
Findings
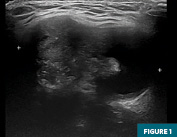
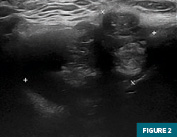
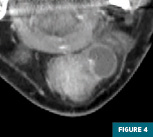
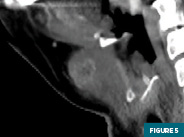
Initial targeted soft tissue ultrasound of the neck at midline demonstrated a 4.6 cm heterogeneous mixed cystic and solid mass at level 1 cervical nodal station (Figures 1 and 2). Subsequent imaging with contrast-enhanced CT of the neck confirmed the presence of a left para-midline enhancing mixed cystic and solid mass with an enhancing mural nodular component. This mass was located slightly inferior to the hyoid (Figures 3, 4, and 5) and was embedded within the strap musculature and clearly deep to the platysma. This mass was concerning for a neoplasm originating from a thyroglossal duct cyst.
The patient was referred to surgical oncology and underwent surgical resection of the left para-midline mass via a Sistrunk procedure. Postoperatively, a dedicated thyroid ultrasound was completed, which demonstrated homogeneous thyroid parenchyma without nodularity or microcalcifications (Figure 6).
Surgical pathology demonstrated a primary 3.5 cm infiltrating papillary carcinoma of the thyroid, classical type, with oncocytic cells component arising in the thyroglossal duct cyst. The margins of resection were free of tumor, and the closest margin was 0.3 mm. Hyoid bone showed normal bone marrow for the age of the patient with no evidence of involvement by papillary carcinoma; pTNM: PT2.
On follow-up, the patient reported that his recovery from surgery was uneventful. He denied dysphagia, dysphonia, or dyspnea. He denied neck discomfort either at the operative site or at the level of the thyroid gland. He was not sure about his family history of thyroid cancer.

Diagnosis
Papillary carcinoma of the thyroid arising in a thyroglossal duct cyst
Discussion
Thyroglossal duct cysts result from remnants of the embryologic thyroid primordium conduit, which fail to obliterate after thyroid migration. They manifest along the midline or para-midline, from the foramen cecum to the thyroid gland. These cysts vary in the epithelial lining, which may include squamous or thyroidal acinar cells. Typically well demarcated, thyroglossal duct cysts appear as anechoic, avascular masses on ultrasound with occasional septations and internal debris. Imaging features on contrast-enhanced CT show low attenuating well-delineated cystic masses with thin walls. Description and distinction of these cysts require their location in relation to the hyoid and the strap musculature. Approximately 50% occur at the level of the hyoid, with the subsequent 25% remaining superior and an additional 25% traveling inferior to the hyoid. Thyroglossal duct cysts should be differentiated from other midline neck masses such as lingual or ectopic thyroid, dermoid/epidermoid cysts, and branchial cleft cysts. Rarely, around 1%, malignant transformation can occur, with papillary carcinoma being the most common subtype, necessitating a thorough evaluation for appropriate management. Given that these malignancies arise from the same duct tract, their locations will mimic that of the benign duct cysts. These malignant transformations are best differentiated from benign cysts with contrast-enhanced CT. They can demonstrate an enhancing mural nodule with additional septal thickening or a complex cystic and solid mass with irregular calcifications. Interestingly, these complex cystic masses could represent metastasis from a primary thyroid papillary carcinoma. Supplemental information may be provided with fine-needle aspiration to differentiate any chance of inflammatory mural thickening from carcinoma. However, a definitive diagnosis requires final pathology. Surgical excision, via the Sistrunk procedure, of the thyroglossal duct cyst and its tract includes additional removal of the anterior third of the hyoid bone and a core of the base of the tongue at the foramen cecum. Recent investigations suggest stepwise increase in surgical excision and even radioiodine ablation depending on sonographic evaluation of the thyroid gland, tumor size, and evidence of metastatic disease.
— Kevin Haines, DO, is a radiology resident at UConn Health.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health.
Resources
1. Agrawal V, Colbert KR, Kumar S, Dharanya -, Bhat RV. Papillary carcinoma of thyroglossal duct cyst—a diagnostic and therapeutic conundrum. Kathmandu Univ Med J (KUMJ). 2023;21(81):106-109.
2. Alatsakis M, Drogouti M, Tsompanidou C, Katsourakis A, Chatzis I. Invasive thyroglossal duct cyst papillary carcinoma: a case report and review of the literature. Am J Case Rep. 2018;19:757-762.
3. Boyanov MA, Tabakov DA, Ivanova RS, Vidinov KN. Thyroglossal duct cyst carcinoma. Endokrynol Pol. 2020;71(3):275-276.
4. Motamed M, McGlashan JA. Thyroglossal duct carcinoma. Curr Opin Otolaryngol Head Neck Surg. 2004;12(2):106-109.
5. Suresh S, Vm P, Thomas S, et al. Papillary thyroid carcinoma arising from thyroglossal cyst—an institutional experience over a decade. Indian J Surg Oncol. 2023;14(1):155-159.

