 On the Case
On the Case
By Joseph Ryan, MD, and Alex Merkulov, MD
Radiology Today
Vol. 26 No. 2 P. 30
History
A 16-year-old male with a past medical history of bilateral maxillary and mandibular third molar extractions presented for CT imaging evaluation of a lesion involving the left hemimandible first identified six months prior. The patient initially experienced mild left mandibular swelling but was otherwise asymptomatic. The patient also has a past medical history of bilateral orchiopexy for right testicular torsion and had undergone arthroscopic repair of a complex lateral meniscal tear with underlying discoid meniscus. Past medical and surgical history were otherwise unremarkable.
Findings
Initial panoramic imaging (not shown) revealed a well-defined, corticated radiolucency associated with the mandibular canal, not definitively associated with a specific tooth, and without a cystic lining seen. The lesion was sampled in April 2024, with two tan-brown soft tissue fragments measuring up to 0.5 cm and 0.6 cm submitted to the oral pathology lab. Macroscopic appearance was consistent with fibrous and cemento-osseous dysplastic elements. Microscopic inspection of decalcified sections revealed fragments of cellular fibrous connective tissue containing delicate trabeculae of viable osseous tissues with entirely benign cytological features. A strip of nonkeratinized epithelium with an aggregate of chronic inflammatory cells in one of the sections was thought to be related to overlying mucosa and the biopsy. Microscopic appearance overall was consistent with a benign fibroosseous neoplasm; when also factoring in the clinical and radiographic features available at that time, the most likely diagnosis was felt to be cemento-ossifying fibroma.
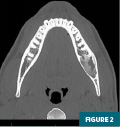
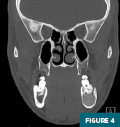
Noncontrast CT imaging of the facial bones and adjacent soft tissues was subsequently performed in November 2024 for presurgical planning with axial, coronal, and sagittal images reconstructed (Figures 1 to 6). CT revealed a partially heterogeneous, predominantly moderately high-attenuation, sharply circumscribed, expansile lesion within the left hemimandible extending to the angle of the mandible and the adjacent mandibular canal. The lesion measured approximately 3.2 cm anteroposterior by 1.6 cm transverse by 1.7 cm craniocaudal and demonstrated contiguity with the roots of the left first and second mandibular molars. The adjacent left third molar was surgically absent. The lesion was noted to show mild, diffuse, concentric cortical thinning. However, no disruption of overlying cortical bone was noted. No abnormalities in the adjacent soft tissues were present.





The patient underwent left marginal mandibulectomy and reconstruction with bone grafting in December 2024. During the surgical excision, the inferior alveolar nerve was identified, partially contained within the specimen, requiring careful removal; the nerve was confirmed intact after excision of the lesion. Intraoperative radiographic imaging of the surgical specimen was performed to verify complete removal of the specimen before closure (Figure 7). Following lesion excision, a left hemimandibular 2.8 mm custom 8-hole titanium reconstruction plate with multiple 2 mm bicortical bone fixation screws was applied, and a combination of artificial bone graft and bone allograft material was placed.
The excised lesion was submitted to pathology as a 5.2 cm segment of slightly tapered bone consistent with mandible, with two smooth resection margins and roughened and jagged margins extending along the superior length of the specimen. The cortical bone was pale tan in color, smooth, and glistening, with minimal pinpoint areas of attached soft, tan tissues.
Microscopic evaluation revealed sections of decalcified tissue fragments of viable bone with normal osteocytes within lacunar spaces. Unremarkable adipose and hematopoietic cells were present within the intervening marrow space, and the surgical margins were negative for tumor. The outside cortical bone was intact and viable. Proliferation of hypercellular fibrous connective tissue partially replaced the central marrow space, with delicate trabeculae of bone osteophyte formation interspersed throughout. All cytologic features in both the soft and hard tissue components were benign, without evidence of malignancy or significant inflammation.
Overall, pathology of the excised lesion was concordant with the imaging appearance and initial biopsy results.
Diagnosis
Cemento-ossifying fibroma of the mandible (COF)
Discussion
COF is a rare, benign, well-differentiated osteogenic solid tumor predominantly containing fibrous tissue, with variable quantities of calcified material that resembles bone and/or cement. The underlying pathogenesis is not entirely known but may be related to congenitally abnormal maturation of dental tissue, which can form bone and cement.
Nomenclature of this entity can be confusing, with COF used as an umbrella term to include the synonymous “ossifying fibroma” and “cementifying fibroma,” which are thought to represent the same entity with differing degrees of central components. Histologically, these tumors can contain both bone (made by osteoblasts) and cement (made by cementoblasts); these cell types share a common progenitor cell origin. In most cases, both materials are present in these lesions, favoring the more general term COF.
The 2005 World Health Organization histological classification of odontogenic tumors classifies them as nonodontogenic. One proposed etiology involves the periodontal ligament, which may account for its relationship to teeth. This classification refers only to “ossifying fibromas,” meant to encompass all of the above-described tumor types. The term COF is generally preferred to distinguish it from noncraniofacial ossifying fibromas, which can occur peripherally throughout the skeleton. Indeed, the characteristic underlying feature of membranous ossification of this tumor limits involvement to the maxillofacial bones, most notably the maxilla and mandible. The most common location is the posterior (molar/premolar) region of the mandible.
Although it can occur in a wide age range, peak incidence is in the second to fourth decades of life, occurring two to five times more commonly in women. It is slow growing and progressive, and can push teeth and adjacent tissues without compromising tooth vitality. Consistency is typically firm, though it can vary depending on the degree of mineralization. The lesions are always covered by normal mucosa, and adenopathy is not typically associated.
Radiographic and CT imaging features include a well-circumscribed mass that expands the bone, gradually growing, initially radiographically lucent/soft tissue attenuation, slowly increasing in attenuation as calcification/ossification occurs during maturation. Expansile morphology with a narrow zone of transition is also seen without cortical breach. On MRI, the lesions are often generally low in signal on T1- and T2-weighted sequences. Soft tissue components in less mature lesions may show mild enhancement.
These lesions are most often identified incidentally or in the context of mild nonpainful swelling. As benign osteogenic tumors, these lesions typically demonstrate slow, gradual progression over time, with little to no risk of malignant transformation. Once diagnosed and adequately characterized radiologically and pathologically, treatment may be considered, especially if there is nerve involvement or cosmetic concern. Treatment is generally surgical, with enucleation and curettage, or wider resection with bone reconstruction for larger lesions.
When these lesions occur in the mandible, involvement of the inferior alveolar nerve can be seen, as was identified intraoperatively in this case, though no associated nerve symptoms were described prior to surgery. Following complete resection, recurrence is generally uncommon, with recurrence rates following resection as low as ~5%. Recurrence after enucleation is slightly higher (~10% to 30%).
A less common variant, the juvenile ossifying fibroma, is a painful, rapidly growing, aggressive tumor found in male children less than 15 years of age. These generally demonstrate a higher degree of cellularity and less indolent clinical picture. Posttreatment recurrence rates are also much higher.
The main differential consideration is monostotic fibrous dysplasia of the jaw. Both can involve the mandible, presenting as a ground-glass attenuation osseous lesion. However, an ossifying fibroma typically shows a thin peripheral border with a narrow zone of transition, as opposed to fibrous dysplasia, which usually has a wider transition zone with the absence of clear delineation between healthy and dysplastic bone tissue in the case of fibrous dysplasia.
Familiarity with COF is important for radiologists, in order to correctly identify and characterize it, as well as differentiate it from similar entities. Radiologic features often help narrow the differential, but pathology typically will confirm the suspected diagnosis. Definitive treatment is usually surgical, with excellent prognosis and low recurrence rates following resection.
Joseph Ryan, MD, is a radiology resident at UConn Health at the University of Connecticut in Farmington.
Alex Merkulov, MD, is an associate professor of radiology at UConn Health.
Resources
1. Curé JK, Vattoth S, Shah R. Radiopaque jaw lesions: an approach to the differential diagnosis. Radiographics. 2012;32(7):1909-1925.
2. Dunfee BL, Sakai O, Pitsey R, Gohel A. Radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics. 2006;26(6):1751-1768.
3. Trijolet JP, Parmentier J, Sury F, Goga D, Mejean N, Laure B. Cemento-ossifying fibroma of the mandible. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128(1):30-33.
